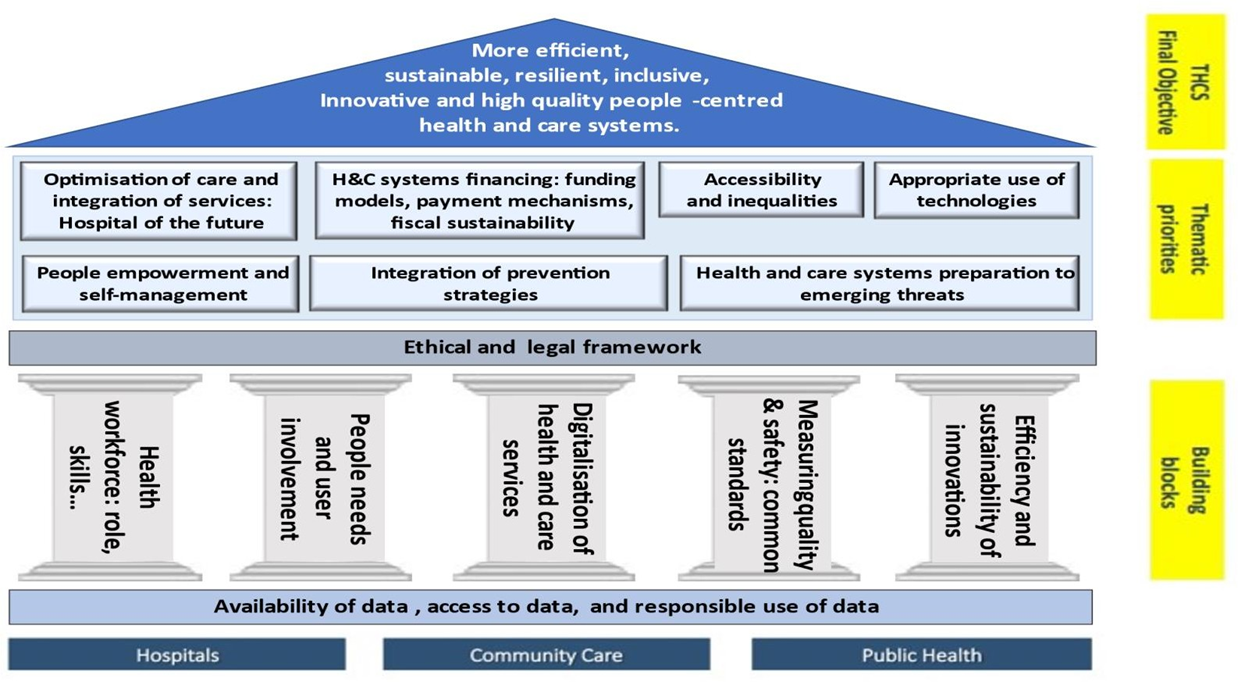
According to its vision and general objective, a key overarching priority of the Transforming Health and Care Systems Partnership is the transition towards more sustainable, efficient, resilient, innovative, and high-quality people-centred health and care systems, inclusive and equally accessible to all people. As such, person- and people-centredness not only requires involving people to explore their needs and become more empowered, but also a system-wide reassessment and redesign of professional orientations and service organisation to adjust to the needs of people and their abilities, rather than the other way around.
To address the increasing challenges and fill the knowledge and innovation gaps and specific objectives, it is important to support research and innovation actions addressing all dimensions of health and care systems:
- Quality of care: safety, effectiveness, patient-centredness, timeliness, efficiency, and equity.
- Accessibility: approachability, acceptability, availability and accommodation, affordability, appropriateness, equity, and one-way entry and navigation in a well-integrated, people-centred and de-siloed system.
- Sustainability: long-term strategic perspective and innovativeness, disease prevention and health promotion, rehabilitation, quality, financial sustainability, institutionalisation of environmental concerns, and institutional accountability and individual responsibility.
- Efficiency: cost-effectiveness and value for money.
- Resilience: knowledge, management of uncertainties, interdependence, legitimacy.
- Inclusiveness: diversity-sensitive, non-discriminatory, stigma-free.
Within the overarching theme of people-centred health and care systems, particular issues are centred around creating conditions that enable people as service users, patients, carers, their families, and communities to play a more central and directing role in their own care as well as in shaping the system that serves them. It also touches upon the implications of personalised medicine for individuals and societies that will have considerable implications for how health and care systems are organised and funded.
Several key questions can be considered while focusing on this overarching priority:
- What are the most effective approaches to engagement that consider people’s values and preferences? These should take into consideration the individual person-professional relationship, the organisation, the co-creation of innovation, the governance and financing, and the wider societal perspective to implementing people-centred strategies.
- What are the most effective investment strategies for supporting the public (e.g. patients, clinicians, or decision-makers) to acquire the skills and abilities for critical engagement, to express their needs and understand risks?
- How do we ensure optimised links between the different tiers of the health and care system to guarantee the systematic and systemic implementation of effective people-centred strategies?
- Which types of measures can best increase health literacy and digital literacy by targeting people and/or health and care professionals?
- How should preventive and curative services be designed for those with lower health literacy and fewer possibilities for self-management?
- How should the potential of health promotion and disease prevention be unlocked by means of concrete strategies, involving multiple actors and sectors?
- What measures are effective to support informal carers?
- What are the skills and contextual conditions needed to deliver personalised medicine, and how will personalised medicine affect health and care in the future?
Consistent with the shift towards more people- and population-centred health and care, a holistic and outcome-based approach that focuses on rigorous measures to assess and improve the quality of health and care is becoming increasingly important.